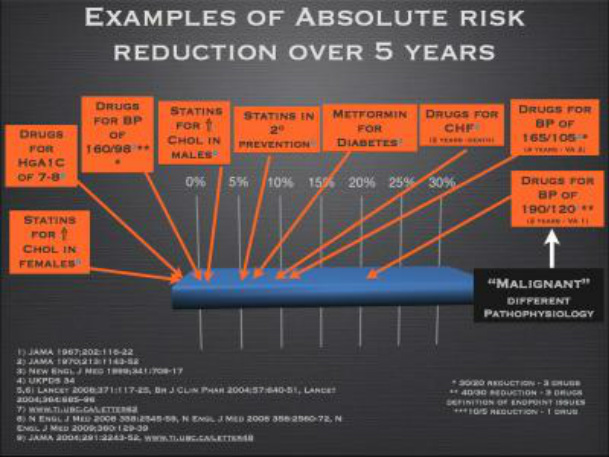
Risk assessment can be done using several tools, the most popular being the Framingham Scale (2) which takes in to account cholesterol levels and calculates a 10 year risk of developing coronary heart disease (CHD)** and more recently a 5 year risk calculator for CVD from the Lancet (3) that is done without the use of cholesterol levels. It is useful to put numbers to the different classifications of risk as each person’s definition of high, moderate or low will vary greatly. Those in the ‘High Risk’ category as defined by Lancet have a 30% or greater chance of developing CVD over a 5 year period. The ‘Moderate Risk’ group using the same scale ranges from a 10-30% chance of CVD over 5 years and the ‘Low Risk’ group has a 5-10% chance of developing CVD in 5 years. The Framingham scale uses similar categories for CHD over a 10 year period creating a baseline risk using your age and modifying that risk depending on several factors listed below. According to this scale, at age 50 your risk starts at 4%, at age 60 your risk is 6% and at 70 years old your risk begins at 10% over the next 10 years. These numbers are a baseline and factors such as gender, high cholesterol levels, smoking, elevated blood pressure, family history of CVD and diabetes will increase your risk accordingly.

Elevated blood pressure is becoming more common as the guidelines are changed and standards lowered and it can be reduced through many interventions including diet and lifestyle changes. One example of past standards is a study published by the Lancet in 1966 which contained patients with an average blood pressure of 200/110 mmHg and the title of that study is “The Effects of Propranolol on MILD hypertension.” If that blood pressure were measured in a patient today they would be sent immediately to the emergency room. It may take time to lower your blood pressure and your readings will vary from day to day so it is best not to measure each day as this may cause stress and elevated readings for some. Two or three readings per month are enough to get an average measurement and a better overview of where your blood pressure truly stands. This article is not meant to defer people from taking their medication. We only wish to inform patients of the actual benefits of their medications. Some may find the risk reduction to be of great value and others may believe that it is not worth the trouble of taking a medication each day (which may come with some unwanted side effects). We support both opinions and encourage patients to make the final decision on their own using all of the information available. Before starting, stopping or altering any of your medications please speak to your health care professional.
*Cardiovascular disease refers to any disease of the blood vessels or heart and includes stroke, heart attack, peripheral vascular disease and coronary heart disease.
**Coronary heart disease refers to blockage of arteries that supply blood to the heart.
***All-cause mortality is defined as death from any cause.
References
1. McCormack, J. and Allan, M. (2008) Therapeutics Education Collaboration Podcast. Episodes 3-12.
2. http://www.framinghamheartstudy.org/risk/coronary.html
3. Gaziano, T., Young, C., Fitzmaurice, G., Atwood, S. and Gaziano, J.M. (2008) Laboratory-based versus non-laboratory-based method for assessment of cardiovascular disease risk. The Lancet; 371:923 – 31.
4. The ALLHAT Officers and Coordinators for the ALLHAT Collaborative Research Group. (2002). Major Outcomes in High-Risk Hypertensive Patients Randomized to Angiotensin-Converting Enzyme Inhibitor or Calcium Channel Blocker vs. Diuretic. JAMA; 288(23):2981- 97.

 RSS Feed
RSS Feed